Preeclampsia and High Blood Pressure During Pregnancy
If you’re Googling symptoms because something feels “off,” or you’re staring at your blood pressure reading wondering if it’s normal-first, take a breath. Preeclampsia can sound scary (and sometimes it is), but understanding the signs and staying informed can make a huge difference. Knowledge isn’t meant to panic you – it’s here so you can feel prepared and supported.
What is Preeclampsia in Pregnancy?
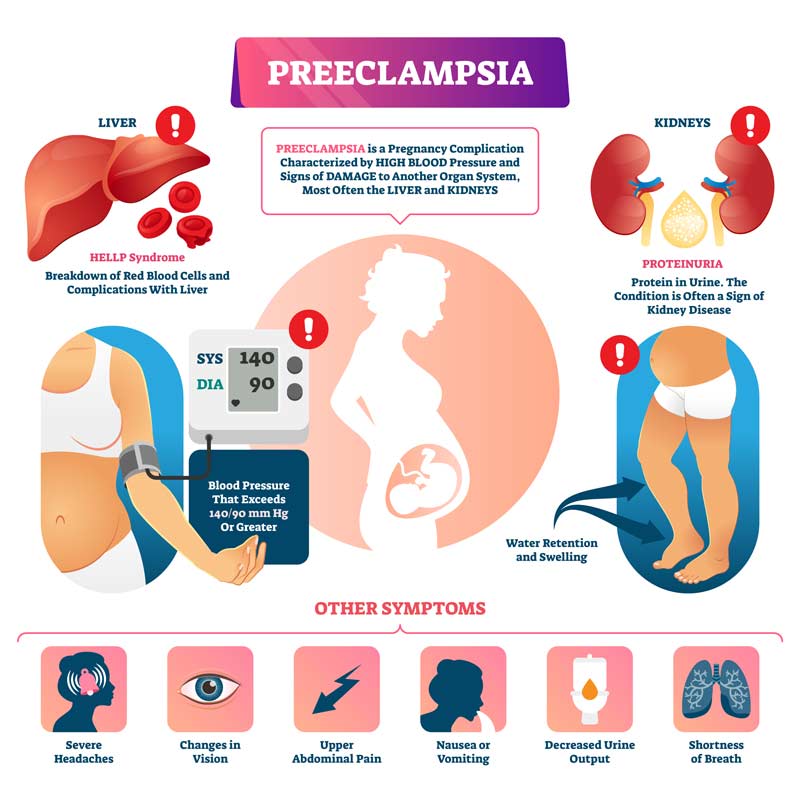
Preeclampsia used to be called toxemia, and it develops when something goes wrong with how the placenta works. This dysfunction causes blood pressure to rise during pregnancy, which can put both mom and baby at risk. It affects about 7 percent of all pregnancies, making it one of the most common serious pregnancy complications. Out of these cases, roughly 1 in 50 women experience a severe form of the condition.
When preeclampsia becomes severe, the risks increase. For the mother, extremely high blood pressure can lead to seizures or other dangerous complications. Low platelet levels may also develop, which can increase the risk of bleeding or hemorrhage. For the baby, the main concern is reduced blood flow from the placenta. When the placenta isn’t delivering enough oxygen and nutrients, the baby may struggle to grow properly or experience stress in the womb.
While the condition can sound scary, understanding the symptoms and seeking medical care early makes a huge difference. With the right monitoring and treatment, many women with preeclampsia go on to deliver healthy babies.
Is Preeclampsia Dangerous?
It can be. High blood pressure during pregnancy isn’t just a number on a chart – it can become life-threatening if it isn’t monitored and treated. With preeclampsia, the elevated blood pressure can slow the flow of blood through the placenta, which means your baby may not get enough oxygen or nutrients. When that happens, it can lead to low birth weight, growth issues, and other complications.
Related: The Placenta – What Is It, Common Positions, and Complications
Am I at Risk of Preeclampsia?
Some women are more likely to develop preeclampsia than others. Your risk is higher if you have a family history of the condition, long-term high blood pressure, kidney disease, pregnancy-induced diabetes, or autoimmune conditions like lupus. Age can also play a role, and women over 40 fall into a higher-risk group.
When Does Preeclampsia Usually Happen?
Preeclampsia typically develops in the second half of pregnancy, often toward the final weeks before birth. However, if there are underlying risk factors, it can appear sooner, which is why regular prenatal checkups are so important.
Who Is More Likely to Develop It?
Family history is a big factor. If your mother or sister had preeclampsia, your chances increase. Women who are overweight (usually with a BMI over 30) are also at higher risk, as well as those at younger or older age ranges – particularly teenagers and women over 40. And if you’ve had preeclampsia in a previous pregnancy, your risk is higher with the next.
Risk Factors for Preeclampsia Include:
- Becoming pregnant as a teen or over 40
- High blood pressure before pregnancy
- Obesity
- Multiple pregnancy
- A past history of kidney disease, high blood pressure or diabetes
- Women who are pregnant for the first time, or who carry more than one child at a time, are more at risk for preeclampsia.
Preeclampsia Symptoms
High blood pressure
Usually defined as a reading higher than 140/90. However, if you normally have low blood pressure, a jump from your normal baseline – even if it’s still below 140/90 – may still be concerning. You can buy blood pressure gauges from your pharmacist if you want to establish your baseline as soon as you know you are pregnant.
Swelling
A certain amount of swelling is normal during pregnancy and you may find it difficult to wear a ring for the full term. Swelling, or edema, that could provoke concern is caused by excess fluid and usually appears in the face, legs, and hands.
Try pressing your thumb into the swelling, if the indentation remains for a few seconds after you remove your thumb, tell the nurse at your next prenatal visit.
Protein in your urine
This is not a symptom you will be able to spot or monitor. You will be tested at each prenatal check-up.
Sudden weight gain
An increase in your weight of more than 2 pounds in a week or 6 pounds in a month will ring alarm bells. If your weight is increasing at that sort of rate, don’t try to diet or lose weight – just mention it at your prenatal appointment so your doctor or nurse can evaluate what’s happening.
Headaches
If you suffer from migraine-like headaches which are not relieved by over-the-counter painkillers (do not take aspirin), contact your doctor immediately.
Vomiting
The nausea that all mothers experience occurs early in pregnancy and goes away. If you experience sudden vomiting in the second half of pregnancy, contact your doctor. Of course, this could just be a bug, but your doctor will check your blood pressure and urine to see if you have other symptoms of preeclampsia.
Early Signs You Shouldn’t Ignore
Some symptoms can feel subtle at first, and many overlap with normal pregnancy changes, which is why monitoring matters. If you notice sudden swelling, persistent headaches, vision changes, or rapid weight gain, it’s worth mentioning to your doctor – especially if the symptoms appear quickly or feel “different” than normal pregnancy discomfort.
Related: Natural Remedies and Tips to Reduce Morning Sickness During Pregnancy
Treatment for Preeclampsia
- Allow frequent monitoring of both you and your baby by your doctor. When a woman has been diagnosed with preeclampsia, it’s very important to monitor the situation closely. Monitoring includes frequent ultrasounds, biophysical profiles, non-stress tests, blood pressure checks, weighting for the mom and checking the amount of protein present in the mom’s urine.
- Go on bed rest, either at home or in the hospital, if it’s too early to deliver the baby. For mild cases of preeclampsia, bed rest at home can be indicated. Bed rest helps increase blood flow to the baby and helps lower the mom’s blood pressure. In case of severe preeclampsia, bed rest at the hospital is likely. Being at the hospital can allow for closer monitoring of both the mom and the baby.
- Take medications prior to delivery to help with preeclampsia. Corticosteroids can help mature the baby’s lungs in case early delivery occurs. Taking drugs, such as hydralazine, can help lower the mom’s blood pressure and prevent preeclampsia from progressing. Your personal doctor will know which medications are best for you and your baby.
- Deliver the baby. Delivery is the only real cure for preeclampsia. If the baby is at or near full term and a woman is diagnosed with preeclampsia, labor may be immediately induced, or a cesarean section scheduled. If it’s too early to deliver the baby, doctors may try to hold off delivery using the other treatments described in this article until delivery is absolutely necessitated.
- Use the drug magnesium sulfate during labor and delivery. For women with preeclampsia, magnesium sulfate can help prevent seizures in the mom during delivery and help increase blood flow to the baby and the placenta. IVs are often used to administer magnesium sulfate to the mom during delivery.
Before taking any supplements, medications, vitamins, or “natural remedies,” make sure to speak with your doctor first. Every pregnancy is different, and what’s safe for one person may not be safe for another – especially with preeclampsia.
Prevention
There isn’t a guaranteed way to prevent preeclampsia, but there are steps your doctor may recommend based on your health history and risk level. Prevention looks different for everyone because it depends on factors like blood pressure, medical history, and how your pregnancy is progressing.
For some women who are considered high-risk, doctors may suggest low-dose aspirin (often referred to as “baby aspirin”). Research shows that taking 81 mg daily after the first trimester may help lower the risk of developing preeclampsia. Some doctors also recommend increasing calcium intake if you’re deficient, since calcium has been shown to help in certain cases.
Lifestyle-based prevention may also play a role, including monitoring blood pressure, eating a balanced diet, staying active (when approved by your doctor), and keeping up with prenatal care.
However, it’s just as important to know what not to take. For example, vitamin E supplements have been linked to an increased risk of preeclampsia during pregnancy.
Very important: Before starting any supplement, aspirin routine, or preventative strategy, even if it seems simple or natural, always speak with your doctor or midwife first.
Healthy Routine Ideas to Help You Support a Healthy Pregnancy
Just a quick reminder before we get into this part: lifestyle changes can’t prevent or treat preeclampsia on their own, and they definitely don’t replace medical guidance. But some healthy habits may support overall blood pressure and help you feel your best during pregnancy. Always check with your doctor before changing your routine.
A few gentle things that may help:
- Stay hydrated. Keeping your fluids up can support blood flow and help your body function smoothly during pregnancy.
- Gentle movement. If your doctor approves, things like walking, prenatal yoga, or swimming can help with circulation and stress.
- Be mindful of salt. You don’t need to eliminate sodium, but reducing heavily processed or salty snacks may help some women feel better.
- Prioritize rest. Sleep, deep breathing, and small stress-reducing routines (like stretching before bed or quiet time with a cup of tea) can make a difference in how your body handles pregnancy changes.
Think of this section like small supportive habits – not pressure, not perfection. Just things that can make you feel a little more grounded during a time when your body is doing a lot.
Frequently Asked Questions
How is preeclampsia diagnosed?
Doctors typically check blood pressure, test urine for protein, and may order bloodwork and ultrasounds to monitor both you and the baby. Diagnosis is based on a combination of symptoms, not just one factor.
Can preeclampsia happen without symptoms?
Yes – and that’s one reason regular prenatal appointments are so important. Some women feel completely fine and still develop preeclampsia silently.
Does preeclampsia always mean early delivery?
Not always. Sometimes doctors monitor closely and try to keep the pregnancy going safely. But in many cases, delivery is the only cure, especially if symptoms become severe.
Can preeclampsia go away on its own?
No – it doesn’t resolve until after birth. Symptoms may continue for a short period postpartum, so monitoring doesn’t stop immediately after delivery.
Is preeclampsia preventable?
There’s no guaranteed way to prevent it. However, some women may be recommended low-dose aspirin or calcium supplements if they’re considered high risk. Always talk to your doctor before taking anything.
Does preeclampsia go away after birth?
For most women, symptoms start improving after delivery, but not instantly. Blood pressure can stay elevated for days or even weeks postpartum, so follow-up monitoring is still important.
Does having preeclampsia mean I’ll get it again in my next pregnancy?
There’s a higher chance, yes, but it’s not guaranteed. Your doctor will monitor you more closely in future pregnancies if you’ve had it before.
Is exercise safe if I’m at risk?
Most gentle movement (like walking or prenatal yoga) is fine, but always get approval from your doctor first, especially if you’re being monitored for high blood pressure or symptoms.
Can diet help manage or prevent preeclampsia?
Diet alone can’t prevent or treat it, but eating balanced meals, staying hydrated, and limiting heavily processed and salty foods may support overall health during pregnancy.
Final Thoughts
Preeclampsia can feel overwhelming because there are a lot of unknowns, and every pregnancy is different. But you don’t have to figure it out alone. Regular checkups, paying attention to your symptoms, and speaking up when something just feels off truly make a difference.
Remember, you don’t need to have everything memorized or know exactly what’s happening at all times. Your job is to stay informed, ask questions, and take care of yourself the best you can – physically, mentally, and emotionally. If you ever feel worried, trust your instincts and reach out to your doctor. You deserve support, answers, and peace of mind.
You’re not just growing a baby – you’re navigating a lot of new information and emotions, too. So be kind to yourself. One day, one step, one appointment at a time, you’ve got this.
Have you announced your pregnancy yet?
If not, here are a few creative ideas for pregnancy announcement:
PREGNANCY ANNOUNCEMENT IDEAS FOR HUSBAND
PREGNANCY ANNOUNCEMENT IDEAS FOR PARENTS AND FAMILY
PREGNANCY ANNOUNCEMENT IDEAS AT WORK